In recent years, the incidence of co-occurring disorders—where an individual experiences both a mental health disorder and a substance use disorder—has seen a sharp rise. Managing Dual Diagnosis has therefore become an increasingly urgent challenge for healthcare professionals, families, and patients alike. The combination of psychological distress and addiction often creates a cycle that is difficult to break without professional, integrated care.
At Roshni Foundation, we believe that recovery is possible when both aspects of the diagnosis are treated simultaneously, not separately. When someone struggling with addiction is also battling anxiety, depression, bipolar disorder, PTSD, or schizophrenia, a specialized approach is required. Our experience with Managing Dual Diagnosis has taught us that understanding the root causes and applying the right combination of therapies is the cornerstone of sustainable recovery.
The complexity of these disorders demands a structured, compassionate, and personalized treatment model. With therapeutic innovations now widely accessible, individuals have a better chance than ever before of leading healthy, substance-free lives. This article presents the top five therapies that are currently most effective in Managing Dual Diagnosis, providing insight into their structure, purpose, and long-term impact.
Integrated Dual Disorder Treatment: A Unified Recovery Path
Among the most highly recommended and evidence-based methods for Managing Dual Diagnosis is Integrated Dual Disorder Treatment (IDDT). This therapy is specifically structured for individuals facing co-occurring disorders and emphasises synchronised care. Rather than splitting treatment for substance abuse and mental health between different programs or professionals, IDDT merges both into one comprehensive plan.
The key advantage of IDDT is that it promotes collaboration among psychiatrists, therapists, case managers, and peer support workers. Treatment plans are long-term and adjusted based on the client’s recovery phase. Unlike short-term detox programs, IDDT builds a sustainable path by addressing both psychological symptoms and substance cravings concurrently. This not only reduces relapse rates but also enhances emotional stability, functional recovery, and life satisfaction.
Through IDDT, patients also develop critical skills for daily living. Whether it’s medication management, social engagement, or coping with trauma, each session empowers the individual to regain control over their mind and body. This therapy is widely implemented across advanced mental health care systems and is increasingly forming the backbone of treatment at leading facilities like Roshni Foundation.
Cognitive Behavioural Therapy: Rewiring the Thought Cycle
Managing Dual Diagnosis often requires untangling deep-seated patterns of negative thinking that fuel both addiction and psychological distress. Cognitive Behavioural Therapy (CBT) is a structured, time-bound therapy that targets distorted thoughts and behaviours by helping individuals recognise, challenge, and replace them with healthier alternatives.
In dual diagnosis cases, someone may use alcohol to cope with feelings of worthlessness or turn to drugs when experiencing anxiety. CBT helps break this association by encouraging awareness and self-monitoring. Clients are taught to identify triggers, respond constructively, and develop adaptive coping mechanisms rather than resorting to substance use.
CBT is especially useful for treating depression, anxiety disorders, and trauma-based conditions in tandem with substance dependence. Its structured format makes it easier to measure progress and modify strategies when needed. According to the National Institute on Drug Abuse, behavioural therapies like CBT play a crucial role in reshaping behaviour, particularly when combined with medication and support networks.
Clients at Roshni Foundation undergoing CBT often report improved self-esteem, better emotional regulation, and a stronger commitment to abstinence. CBT’s dual focus on the psychological and behavioural sides of addiction makes it one of the most effective tools for Managing Dual Diagnosis.
Dialectical Behaviour Therapy: Mastering Emotional Balance
For those with intense emotional fluctuations or chronic trauma, Managing Dual Diagnosis becomes especially difficult without emotional regulation strategies. Dialectical Behaviour Therapy (DBT), an extension of CBT, introduces mindfulness, distress tolerance, and interpersonal effectiveness into the recovery journey.
DBT focuses on helping individuals stay present, manage emotional pain without turning to substances, and interact more effectively with others. It is often used in cases where substance use is triggered by emotional crises, relationship instability, or childhood trauma. Unlike other therapies, DBT acknowledges that two seemingly opposite truths can coexist—for example, accepting yourself while still needing to change.
Through individual therapy, group skills training, and coaching, DBT gradually builds resilience. Clients learn how to ride the waves of emotional discomfort without self-destructive behaviour. In dual diagnosis treatment, this often translates into reduced cravings, fewer relapses, and improved mental health stability.
Managing Dual Diagnosis through DBT has shown outstanding results, particularly in individuals with borderline personality disorder, PTSD, and substance abuse. At Roshni Foundation, DBT is one of the core pillars of treatment, helping clients build not just mental balance but also lasting recovery habits.
Motivational Interviewing: Awakening the Desire to Change
One of the most overlooked challenges in Managing Dual Diagnosis is denial or resistance to treatment. Many individuals are not immediately ready to give up substance use, especially if it’s been their way of coping with anxiety, depression, or trauma for years. Motivational Interviewing (MI) is designed to overcome this barrier by engaging clients in a non-confrontational conversation about change.
Unlike directive approaches, MI meets the person where they are emotionally and empowers them to explore the consequences of their behaviour. It encourages self-efficacy, autonomy, and internal motivation—all critical factors in sustained recovery. The therapist acts more like a guide than an authority, helping the client uncover their personal reasons for seeking change.
This makes MI particularly valuable in early recovery, as it often precedes more intensive therapies like CBT or IDDT. At Roshni Foundation, Motivational Interviewing is woven into every stage of recovery, ensuring clients feel respected, heard, and engaged in their healing process.
MI’s contribution to Managing Dual Diagnosis lies in its ability to gently dismantle ambivalence. Once a person feels seen and supported rather than judged, they become more open to addressing both their addiction and mental health challenges.
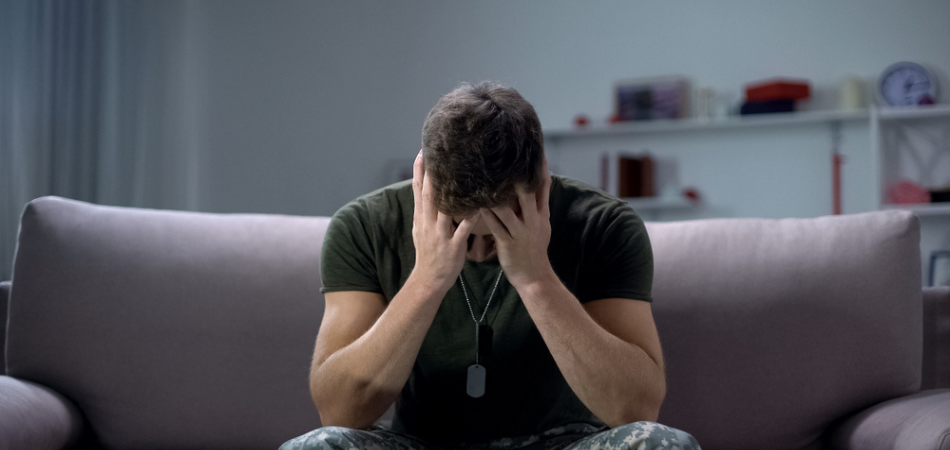
Trauma-Informed Therapy: Healing the Invisible Wound
A significant number of individuals facing co-occurring disorders have a history of trauma, be it childhood neglect, abuse, violence, or grief. Without directly addressing this trauma, any attempt at Managing Dual Diagnosis is likely to fall short. Trauma-Informed Therapy focuses on safety, trust-building, and empowerment, ensuring that treatment does not re-traumatise the individual.
This therapeutic approach does not follow a one-size-fits-all model. Instead, it adapts based on each person’s trauma history and emotional capacity. Techniques may include narrative therapy, EMDR (Eye Movement Desensitisation and Reprocessing), or somatic therapies. The goal is not only to reduce trauma-related symptoms like flashbacks or panic attacks but also to heal the underlying emotional pain that fuels addiction.
At Roshni Foundation, every staff member is trained in trauma-informed care. From the first point of contact to post-rehab support, the environment is intentionally designed to be non-judgmental, predictable, and empowering. This sensitivity is vital for individuals who have never felt safe enough to confront their past, let alone their addiction.
Trauma-Informed Therapy helps reframe the client’s understanding of their behaviours. Instead of asking, “What’s wrong with you?” it asks, “What happened to you?” This simple shift lays the foundation for real transformation in Managing Dual Diagnosis.
Conclusion
Managing Dual Diagnosis requires a multifaceted and deeply empathetic approach. Whether it’s through Integrated Dual Disorder Treatment, Cognitive Behavioural Therapy, Dialectical Behaviour Therapy, Motivational Interviewing, or Trauma-Informed Therapy, each modality offers a unique doorway to healing. When used in combination, they address the mental, emotional, behavioural, and social aspects of co-occurring disorders, laying the groundwork for long-term recovery.
For individuals and families seeking comprehensive care, the best de-addiction centre in Dehradun, Roshni Foundation, offers an integrated treatment plan tailored to each client’s needs. Our commitment to dual diagnosis recovery goes beyond detox—we nurture personal growth, emotional strength, and social reintegration. With the right support, recovery is not only possible—it’s powerful.